The Truth about Dental Insurance
Originally posted by my colleague Dr. Mac Lee on October 4, 2011.
Forty years ago, dental insurance benefits averaged $1,000, which was the equivalent of around $8,000 today. Here is the kicker; the average insurance plan is still close to $1,000. The purpose of this article is to explain the facts and fiction of what everyone calls “dental insurance.”
Fiction:You have a major medical problem, which includes surgery and hospitalization. You expect your insurance to take care of the major expenses after the deductible, and it does so. You would think dental insurance works the same way, but it doesn’t. Just calling it insurance is complete and total fiction.
Fact: People who think they have dental insurance really only have limited and restricted benefits that are controlled by an insurance company. A dental benefit is more like a coupon. It is only worth what the insurance company says its worth. It has nothing to do with what the dentist charges.
Fiction: To believe these two statements are true “My dental insurance will pay for it,” or “My dental insurance will pay 80 percent” is, in fact, fiction.
Fact: $1,000 was a lot of money when I graduated from dental school in 1972. That year, we bought a brand new Buick for $3,000. My crown fees were $250 and the insurance company paid well. Basically, a patient could get two or three crowns a year on old broken down, filled teeth and in a few years, their mouth was fixed. Plus, the patient could get two cleanings a year and not even max out their insurance. It was a great deal for patients and dentists.
If benefits kept up with inflation and raised the benefit ceiling each and every year with today’s benefit close to $8,000, people would still have a good deal. As it is, today’s crown price for one tooth will basically wipe out a year’s benefit. Not only that, the insurance company (yep, the one with the skyscrapers in New York, Chicago and San Francisco) often goes out of its way to deny your benefits.
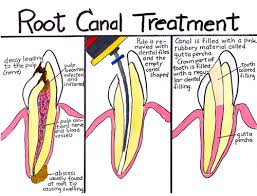
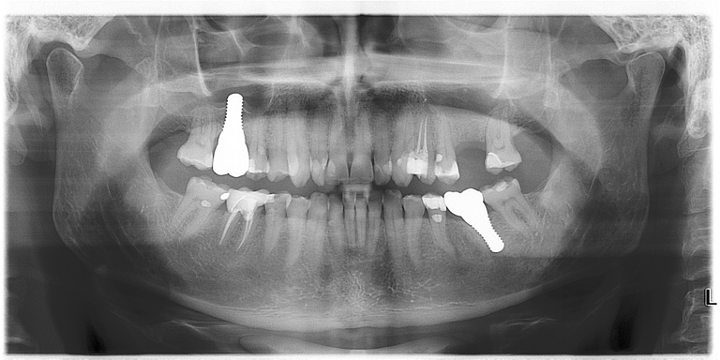
Fact: Today’s dentistry is nothing like it was 40 years ago. If patients had problems, the choices were to pull, fill or crown. Today’s dentistry serves the patients with some of the most advanced, pain-free techniques in medicine. These procedures are not even covered by the dental benefit contract, or the procedures cost more than the paltry yearly benefit.
Back then, there was no such thing as Managed Care. Today’s insurance companies want you to choose a dentist based on cost and assume that all doctors are equally talented, knowledgeable, caring, ethical, available and personable – and that just isn’t true. The dentist making the deal with the insurance company may take a cut up to 30 to 50 percent. In order for them to stay in business, they have to see more people, do more procedures and cut costs in some manner. And even though it is a managed care system, dental benefits still acts as a coupon and not insurance.
Fiction: The dentist and dental team should understand a person’s dental benefit, what it will cover, pay, etc.
Fact: The contract is between the employer, employee and insurance company. The dentist has no role to play whatsoever; they are simply caught in the middle. Dentists, as a whole, are great people who love to help others. They try very hard to accommodate by hiring extra staff just to handle the paperwork, phone calls, etc., that insurance companies require.
Most important: Never let an impersonal insurance company dictate your dental care. They couldn’t care less about your health, comfort, peace of mind or appearance. Be happy you have that coupon for some dollars off, but never expect them to rebuild your burned-down house.
Mac Lee is a dentist in practice in Edna. He is the co-founder of Dentists Who Care, a national movement to educate the public on modern dentistry.
If you have any questions about your insurance feel free to contact our office at 1 613 376 6652 or visit our website at www. ClintonDentistry.com